Analyze multi-slice exams with AI that highlights suspicious findings, speeds up review, and reduces reading fatigue.

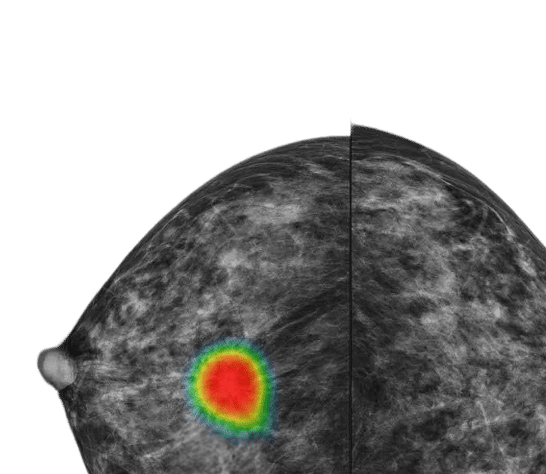
Lunit INSIGHT DBT (3D) AI-powered mammography software enhances lesion detection in digital breast tomosynthesis exams, helping radiologists interpret complex cases with greater precision.
It delivers AI-guided navigation during image review and is built for seamless integration into PACS and viewers. This reduces reading time*, simplifies slice selection, and supports single and double-reading workflows, helping manage high case volumes and reduce radiologist fatigue.
*Eun Kyung Park, et al., Impact of AI for Digital Breast Tomosynthesis on Breast Cancer Detection and Interpretation Time, Radiology Artificial Intelligence, 2024.
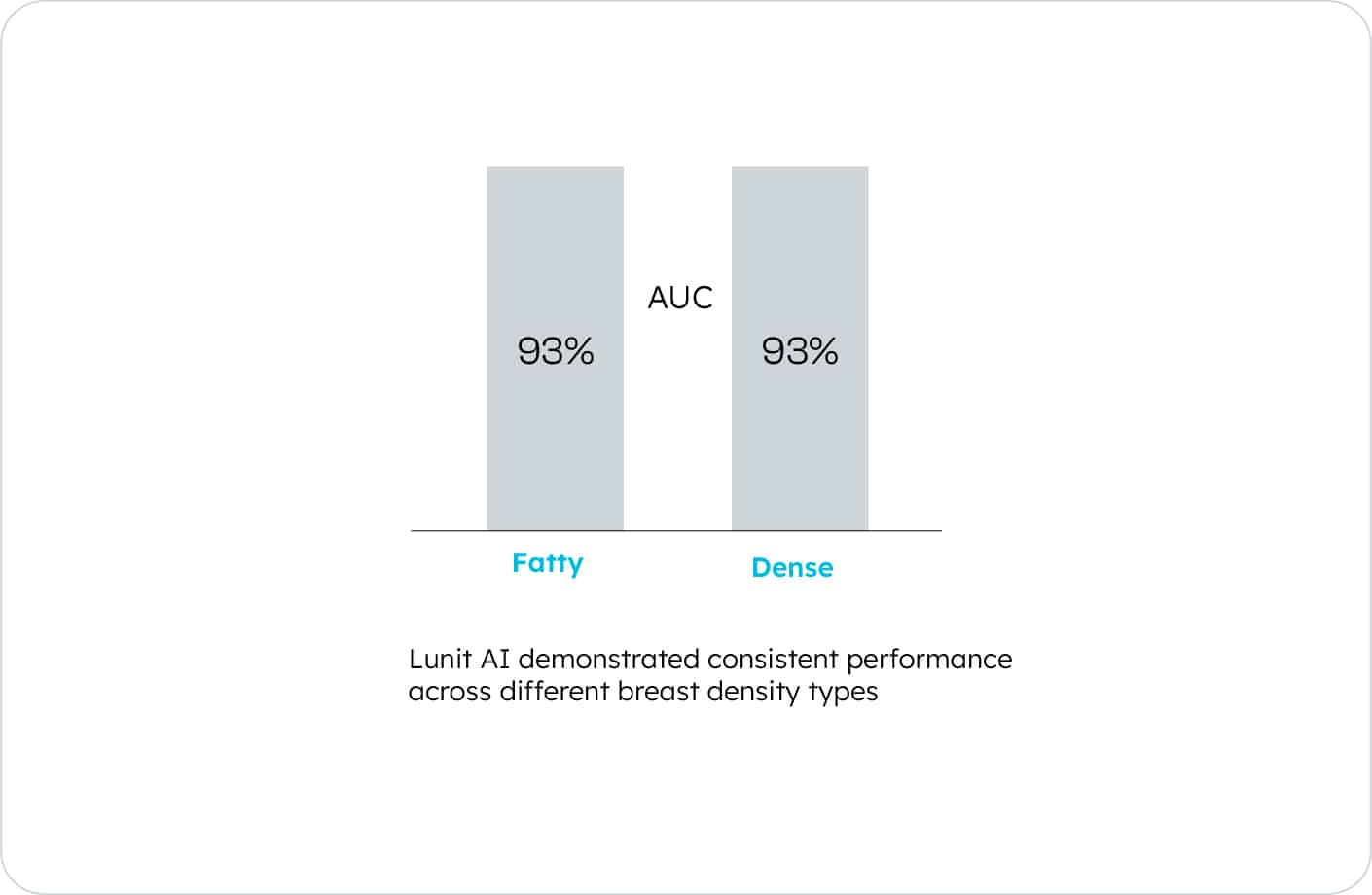
Lunit INSIGHT DBT enhances breast cancer detection in both fatty and dense breasts. By supporting more consistent interpretation across tissue types, it helps radiologists catch subtle or early-stage cancers that are often missed in standard screening.¹
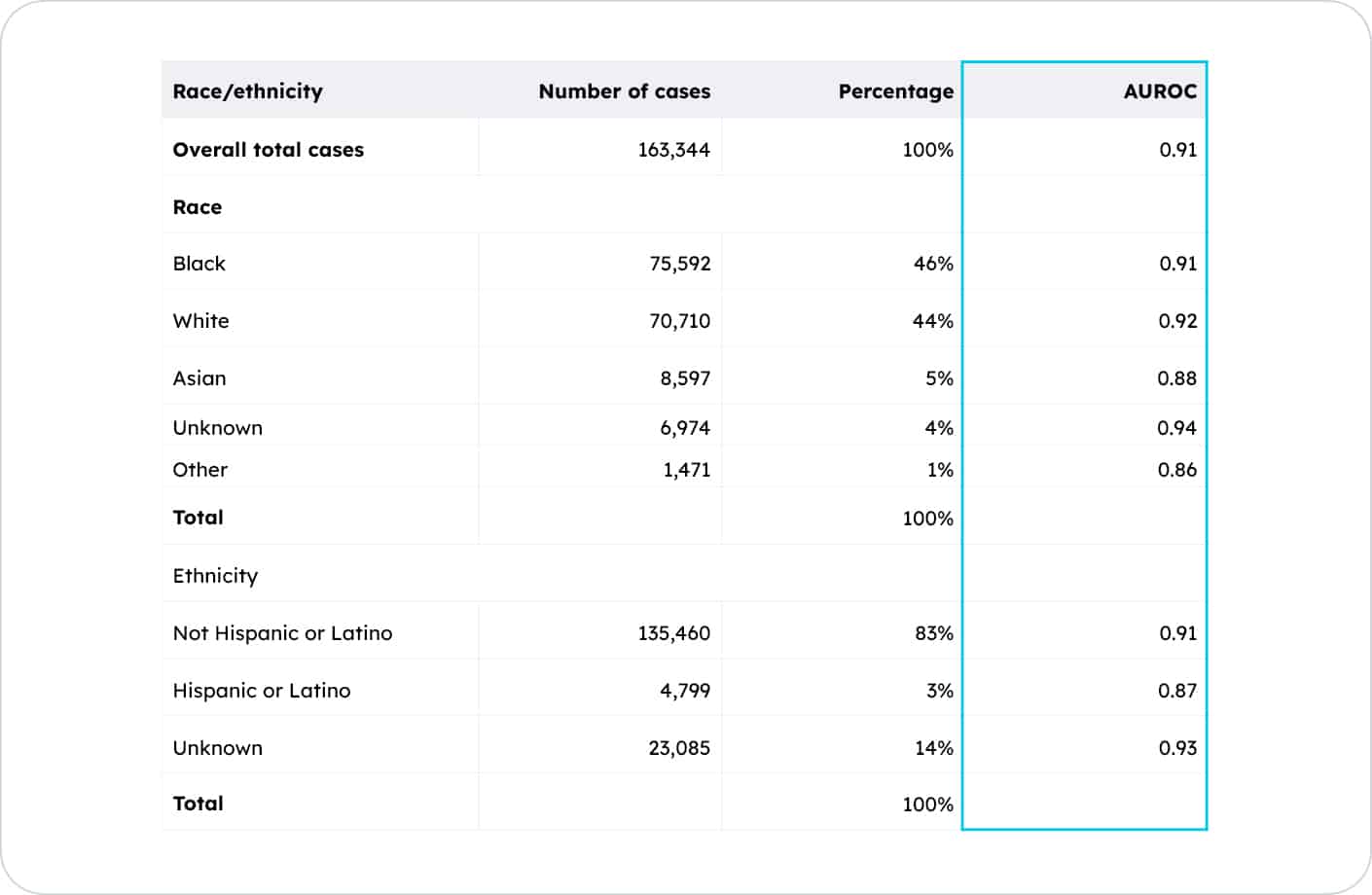
Trained on diverse datasets from the US, UK, and Korea, Lunit INSIGHT DBT delivers robust performance across patient demographics. In an Emory study* of 163,000+ DBT exams, results were consistent across racial and ethnic groups, supporting more equitable screening outcomes.
*Mulry BB et al, Performance of a Commercial Digital Breast Tomosynthesis Model for Breast Cancer Detection by Demographic, Imaging, and Pathologic Subgroups. Preprint (2025), 1-13.
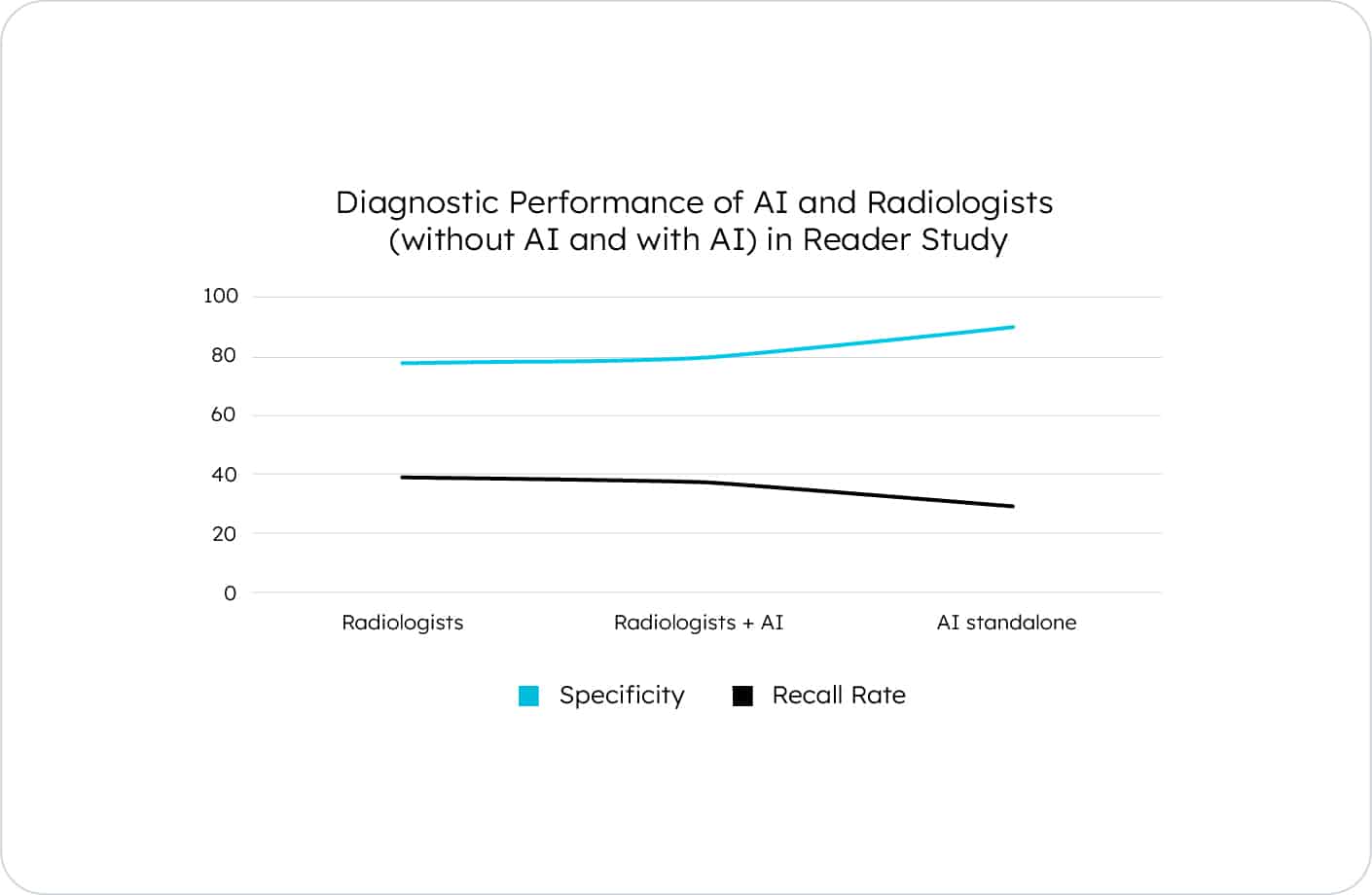
With improved specificity, Lunit’s AI helps reduce unnecessary recalls*, supporting more confident reads and lowering patient anxiety. Radiologists can interpret DBT exams with fewer interruptions and clearer decision support.
*Park EK et al, Impact of AI for Digital Breast Tomosynthesis on Breast Cancer Detection and Interpretation Time. Radiology Artificial Intelligence, Volume 6: Number 3 - 2024.
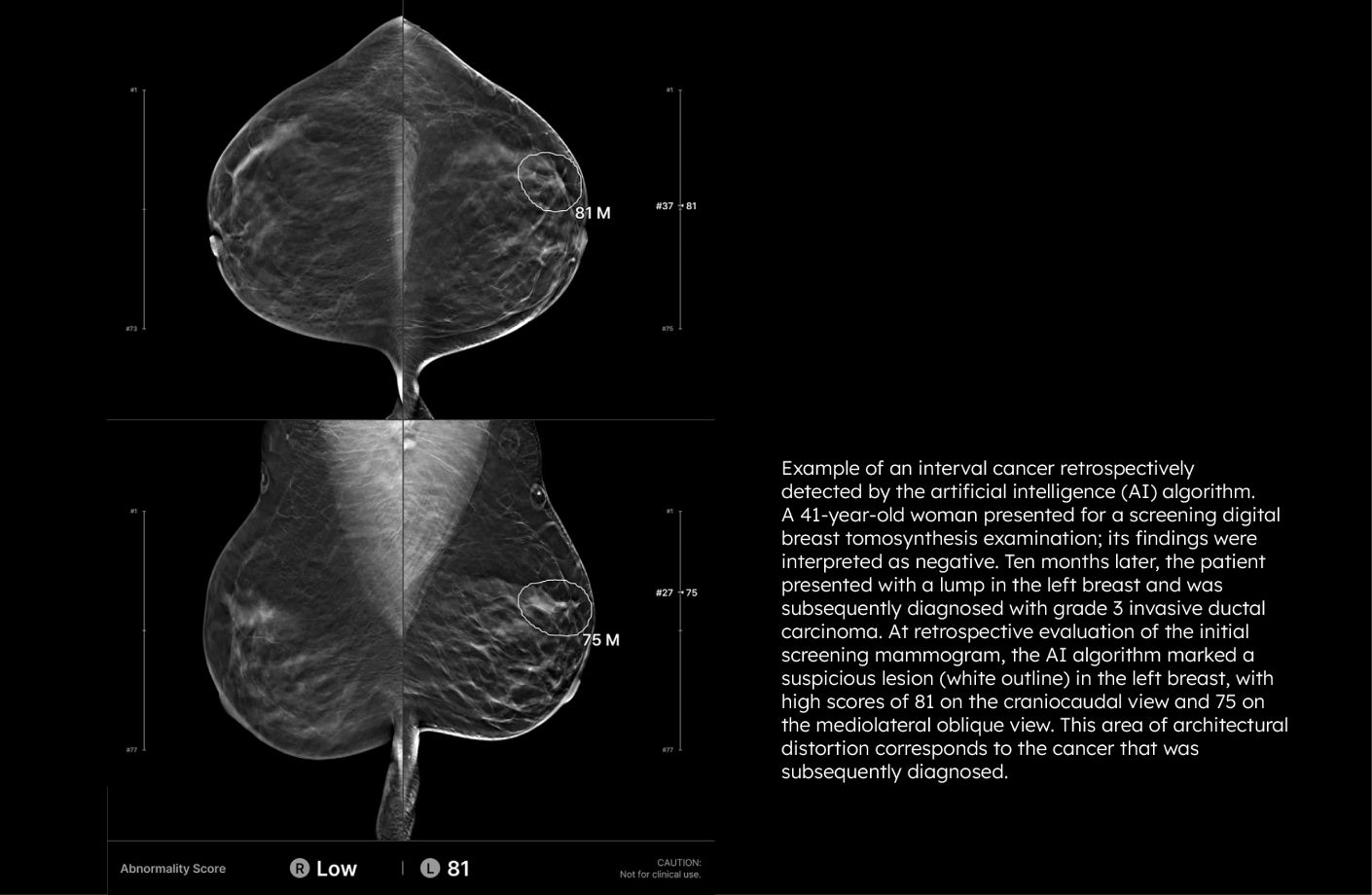
Lunit INSIGHT DBT correctly localized nearly one-third of interval cancers in a recent study*, many of which were large or more advanced. By identifying these earlier, AI can help improve DBT screening outcomes and potentially reduce breast cancer-related mortality and morbidity.
*Bahl M, Langarica S, Lamb LR, et al. AI to Reduce the Interval Cancer Rate of Screening Digital Breast Tomosynthesis. Radiology. 2025
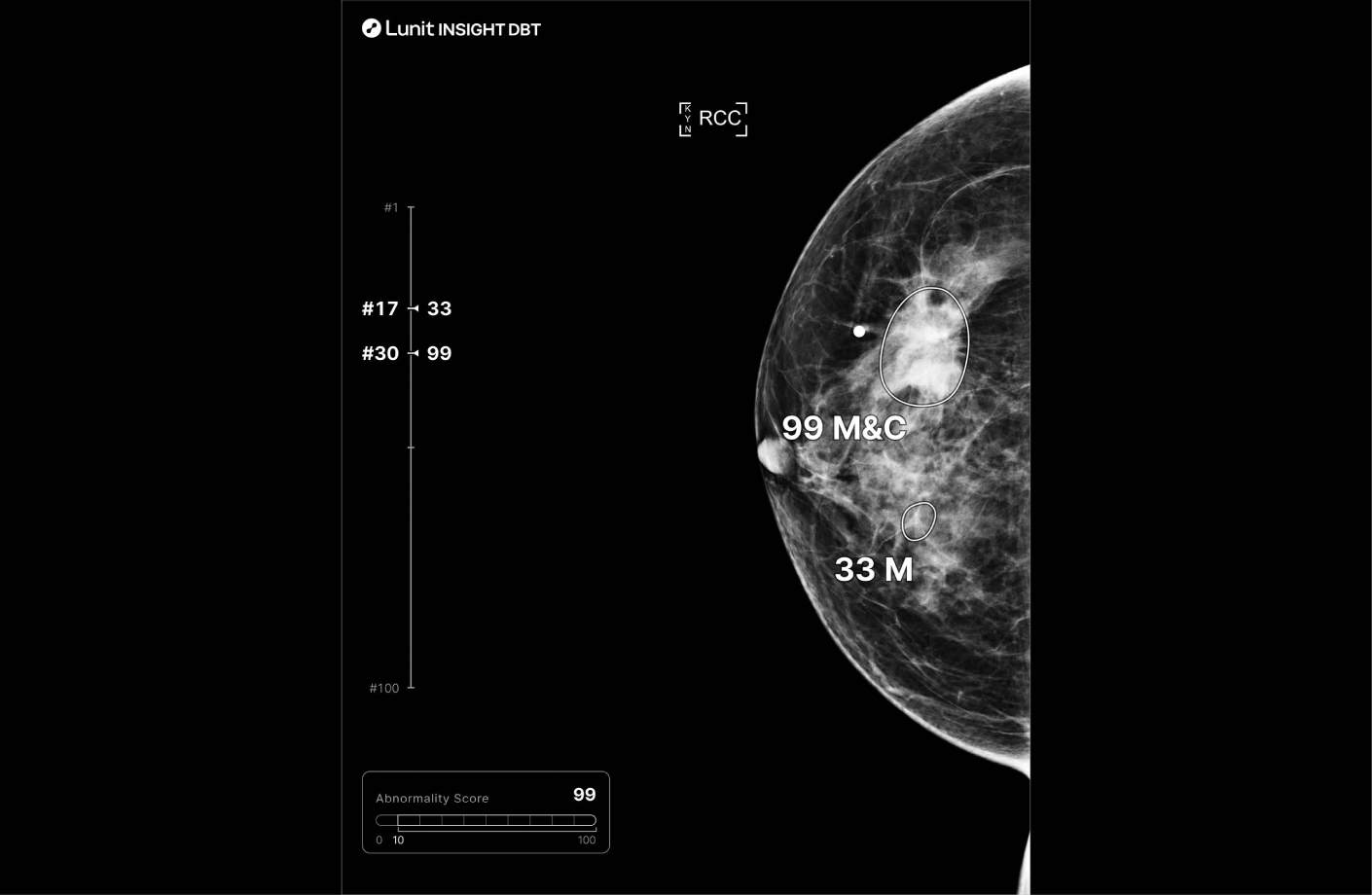
Each suspicious lesion is assigned an abnormality score (0–100), helping quantify malignancy likelihood. Location is clearly marked using heatmaps or contours, and lesion types—such as masses (including architectural distortion and asymmetry), and calcifications—are identified for targeted interpretation. The best slice for lesion visualization is marked on the navigation bar for quick review.
Stay informed with the latest research, product updates, and global partnerships driving innovation in AI-powered cancer screening.
Explore clinical briefs, product guides, and tools designed to help you optimize your use of Lunit’s AI-powered mammography software for digital breast tomosynthesis.
